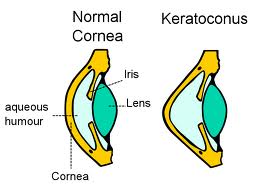
Keratoconus is a progressive eye disease that thins the area around the cornea, leading it to bulge into a cone shape that deflects light when it enters the eye and projects onto the retina. This can distort the vision. The symptoms of this condition typically begin in the teens or early 20s. New research has suggested that this condition is caused by an enzyme imbalance in the cornea that leads to oxidative damage and free radical damage.
Some have a genetic predisposition to keratoconus but overexposure to UV rays, wearing poorly fitting contact lenses for a long period of time, constantly rubbing the eyes and chronic eye irritation can also cause this condition.
Symptoms of Keratoconus
As the cornea's shape alters it will cause the patient to develop an irregular astigmatism to develop nearsightedness. This will increasingly blur and distort the vision over time and may cause sensitivity to light and glare. You may find that your prescription changes every time you visit your eye doctor as keratoconus takes hold.
Treatments for Keratoconus
During the initial stages of keratoconus, soft contacts or eyeglasses can help to manage the symptoms. However, as the cornea becomes thinner and takes on an irregular shape these remedies will no longer be effective. At this point more advanced treatments will become necessary.
1. Gas Permeable Contact Lenses
Those who are having trouble controlling their keratoconus symptoms often turn to GP lenses that allow light to vault over the cornea to correct the shape. These may be uncomfortable to wear and finding a lens that fits properly can be somewhat time consuming. Those who require GP lenses will need to work with their doctor to continually correct the shape of your prescription to address the changing nature of your symptoms.
2. Customized Soft Contact Lenses
Manufacturers are now able to create customized contact lenses that can help to manage mild to moderate kratoconus with less discomfort than gas permeable lenses. KeraSoft and NovaKone lenses are frequently recommended for U.S. patients because they have a wide range of parameters and are larger in diameter which offers a higher range of stability.
Custom fitted lenses can be a more comfortable solution for those that have trouble wearing lenses full time. They can be worn while driving or at work when you may not be able to wear gas permeable lenses. Customized lenses may be more expensive than other types of lenses but vision insurance policies often cover much of this added expense.
3. Piggybacking Contact Lenses
Because GP lenses tend to be uncomfortable for keratoconus patients to wear, some doctors fit patients with two contacts that can be worn over each other in the same eye. This allows you to place a more comfortable soft contact lens on the eye and a GP lens on top to correct the vision. The soft lens acts as a cushion while the GP lens ensures that the eye is receiving an adequate amount of oxygen.
4. ClearKone Hybrid Contact Lenses
Hybrid lenses offer a soft peripheral "skirt" with an oxygen permeable center. This helps to keep the eye comfortable while offering an increased amount of vision correction. A wide variety of parameters are available to help address the irregular shape caused by keratoconus.
5. Scleral and Semi-Scleral Lenses
These lenses are larger diameter GP lenses that reach the edge of the sclera. These vault over the irregular cornea so they do not put pressure on the eye that can cause discomfort.
6. Intacs
These are corneal inserts that are surgically applied beneath the surface of the eye. They sit along the periphery of the cornea to help correct the shape and restore your vision. This surgery has been found to allow the patient to read two additional lines on an eye chart.
7. Corneal Crosslinking
This procedure helps to halt the bulging of the cornea associated with keratoconus. Epithelium-off crosslinking removes the outer layer of the cornea so that riboflavin and UV light can enter more easily. Epithelium-on crosslinking leaves the corneal surface intact, requiring more time for riboflavin to fully penetrate the cornea. Some prefer this surgery because it is less uncomfortable, the recovery time is shorter and there is less risk of infection.
Clinical trials of the crosslinking process are ongoing, but initially imply that this procedure reduces the need for corneal transplants in those that have keratoconus. This may also be an ideal way to prevent complications of LASIK surgery. A combination of crosslinking techniques and Intac implants also appear to be an effective treatment method that does not cause a large amount of complications.
8. Topography-Guided Conductive Keratoplasty
During this treatment radio waves are applied to points around the periphery of the cornea with a probe to reshape the surface of the eye. Individual plans for this procedure can be created with digital mapping. Initial study of this method indicate that this procedure can help to eliminate irregularities in the surface of the cornea.
9. Corneal Transplant
Those who have trouble managing rigid contact lenses or have keratoconus that has progressed to a point where corrective lenses cannot correct their vision may require a corneal transplant. This is considered to be the last resort for treatment and may not completely erase vision problems in the patient.
For more treatments on keratoconus, see what doctor has to say: